Delaware Imaging Centers
Delaware Imaging Network (DIN) is a comprehensive diagnostic imaging network, formed in 2018 by two of Delaware’s premier imaging providers – Papastavros’ Associates Medical Imaging (PAMI) and Diagnostic Imaging Associates (DIA).
We provide expert care and cutting edge technology including MRI, PET/CT, CT, 3D Mammography, Ultrasound, Nuclear Medicine, Fluoroscopy, X-ray, DEXA | Bone Density and more.
Our collaborative network of outpatient imaging centers have delivered quality and convenience to local and neighboring communities in Wilmington, Newark, Dover, Glasgow, Middletown, and Milford for over 50 years. With continued dedication to the care and comfort of our valued patients, we are proud to offer imaging services at costs much lower than hospital owned imaging centers.
Trending Radiology
Recent Radiology News
Radiology Services by Location
See what imaging services are performed at each of our locations.
Imaging Centers Near You

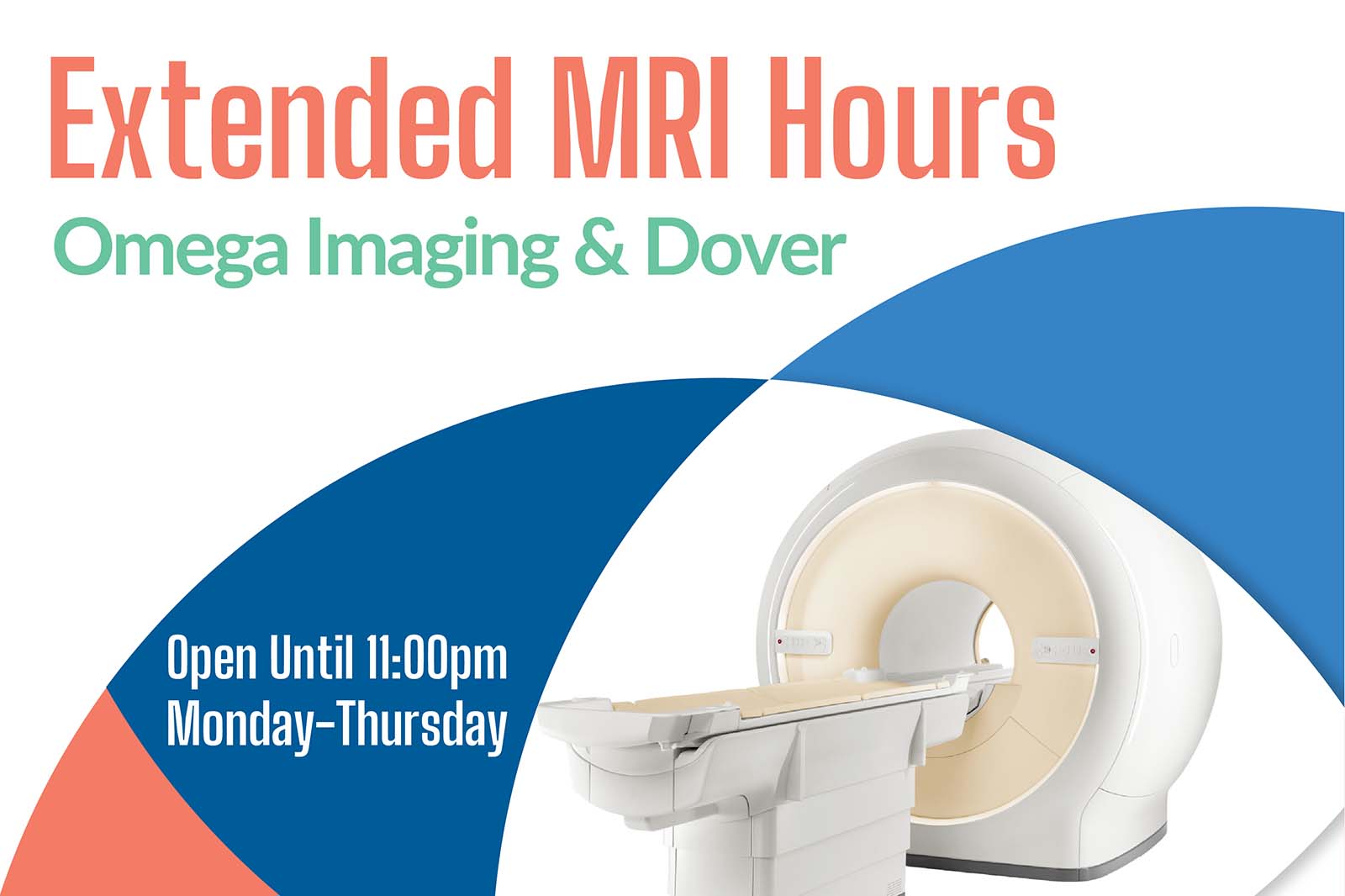
Flexible exam hours designed around your schedule.
Radiology appointments available on your terms.